Risk-reducing surgery
Risk-reducing surgery (also known as preventative surgery or prophylactic surgery), is a form of surgery whose purpose is to minimise or prevent the risk of developing cancer in an organ or gland. For women at high risk, risk-reducing surgery includes bilateral mastectomy and salpingo-oophorectomy.
Risk-reducing mastectomy
A risk-reducing mastectomy is surgery that removes one or both healthy breasts. It is offered to women who have a very high risk of developing breast cancer due to a genetic mutation or if there is a strong family history of breast cancer (but no genetic predisposition).
The Belgian guidelines on risk management recommend bilateral risk-reducing mastectomy for women with one of the following genetic mutations: BRCA 1, BRCA 2, PALB 2 and ATM. For women with a mutation in the CHEK 2, RAD51C and RAD51D, BARD1 genes, risk-reducing mastectomy is recommended if there is a strong family history or if diagnosed with breast cancer. For women who carry a TP53 variant, current guidelines recommend that the option of risk-reducing mastectomy be discussed on a case-by-case basis.
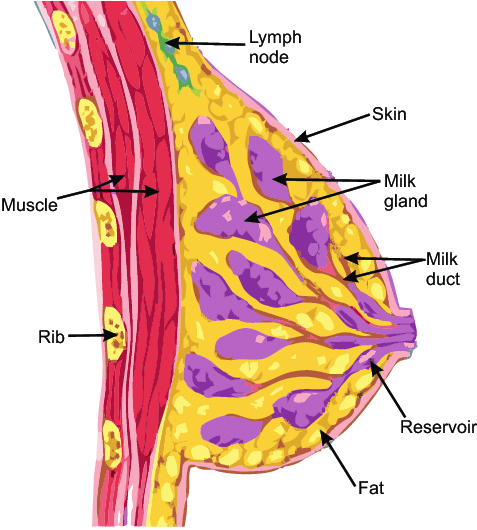
Source: Swierzewski, 2017
For high-risk women who have not developed the disease, a bilateral prophylactic mastectomy can drastically lower breast cancer risk by 90-95% or more. For high-risk women who have already been diagnosed with breast cancer, this surgery can help reduce the risk of developing a second breast cancer. For both groups of women, in practice It is impossible to completely eliminate the risk as it is not possible to remove all breast cells, so a small risk of developing breast cancer after a risk-reducing mastectomy (2-5%) still remains.
A prophylactic mastectomy is a permanent and irreversible procedure. If you plan to have children, you must therefore consider that the operation prevents breastfeeding. In addition to genetic risk, factors such as age, other medical conditions, lifestyle, and mental health will be taken into consideration when determining whether or not to have a prophylactic mastectomy.
Women who undergo a mastectomy have the option of either reconstructing the shape of the removed breasts, or going flat through an aesthetic flat closure (no reconstruction). Women who choose to have their breasts reconstructed have several options. The breast can be reconstructed using implants (saline or silicone). They can also be reconstructed using autologous tissue (i.e. tissue from other parts of the body). Sometimes both implants and autologous tissue can be used to reconstruct the breast. Surgery to reconstruct the breast can be performed (or started) at the time of the mastectomy (called immediate reconstruction) or it can be performed at a later time (called delayed reconstruction). Delayed reconstruction can occur months or even years after the mastectomy.
Undergoing a mastectomy remains your personal choice. High-risk women who decide not to undergo this surgery may still opt for frequent radiological screening.
Risk-reducing salpingo-oophorectomy
To date, there is no effective screening method for ovarian cancer. The only radical preventive approach is to perform a bilateral salpingo-oophorectomy (BSO), which is the surgical removal of healthy ovaries and fallopian tubes. This surgery is the most effective way to reduce risk in these tissues, to levels below 5%. For women with a BRCA 1 mutation, bilateral salpingo-oophorectomy is recommended by age 40. For those with a BRCA 2, PALB 2, RAD51C, RAD51D, or BRIP 1 mutation, surgery is recommended by age 50, but family history needs to be evaluated.
There are two main surgical methods for removing the ovaries: keyhole (laparoscopy) or open surgery (laparotomy). Both are performed under general anaesthesia. In most cases, the surgery is performed using laparoscopic (keyhole) surgery.

Source: Swierzewski, 2017
A “two-stage” preventive intervention called risk-reducing salpingectomy with delayed oophorectomy (SDO), may be offered to women who refuse to have their tubes and ovaries removed at the same time. This operation consists in the initial removal of the fallopian tubes (salpingectomy) to reduce the risk of disease and allow the maintenance of ovarian function and therefore avoid effects related to early menopause. At a later point in life, the ovaries will be removed (oophorectomy) to complete the 1st surgery and minimise the risk of ovarian cancer. Studies and clinical trials regarding the effectiveness of this approach are ongoing. Check our trials page.
Monitoring after prophylactic surgery is an annual consultation with your gynaecologist.
Removal of the ovaries carries some side effects, specifically loss of fertility and the onset of premature menopause. This operation in fact causes an instant surgical menopause. Menopausal symptoms can vary from one woman to another. Some women may have no menopausal symptoms after surgery, others may have some, such as hot flushes, night sweats, tiredness, loss of libido, vaginal dryness, and mood changes. Women who undergo a bilateral salpingo-oophorectomy before age 50 are usually offered Hormone Replacement Therapy (HRT) to prevent symptoms of menopause and to protect their overall well-being (including heart and bone health). The use of HRT after a risk-reducing salpingo-oophorectomy needs to be carefully discussed with your medical team, especially if you have had or have breast cancer.
Bilateral salpingo-oophorectomy also causes loss of fertility. For information on fertility and family planning, consult the dedicated page.

We can support you in various ways:
- Contact us via our helpline
- Join our online community group
- Contact one of our buddies
- Read the testimonials

 BRCA+ Network asbl
BRCA+ Network asbl